Introduction 🔗
If you work in the medical device space, by now you probably know that FDA is cracking down on cybersecurity. You’ve probably heard horror stories from other friends in industry about pen testing, threat modeling, SBOMs, and the like.
How do you avoid slowing down your FDA marketing submission (510(k), De Novo, or PMA) with cybersecurity problems? You can read the guidance documents (or hire us), but you will also do well to avoid the 14 common cybersecurity deficiencies listed in the article.
In this article, we will discuss 14 common cybersecurity deficiencies found in FDA AINN letters. It includes quotes taken from recent FDA clearances with proprietary details, such as K numbers, page numbers, and other irrelevant items removed.
We have seen these deficiencies on multiple FDA submission. If you fail to address these issues, you will likely get similar responses on yours. If you know what questions FDA is going to answer before they ask them, you will have a leg up in your FDA submission, such that you may address the answers to these questions even before FDA asks them.
What is an AINN Letter? 🔗
When you submit a 510(k), De Novo, or PMA to FDA, they will often respond with a list of major and minor deficiencies. This information is communicated in what is called a “letter for additional information,” often abbreviated AINN. It is also known as an AI letter or hold letter.
Common FDA Deficiences 🔗
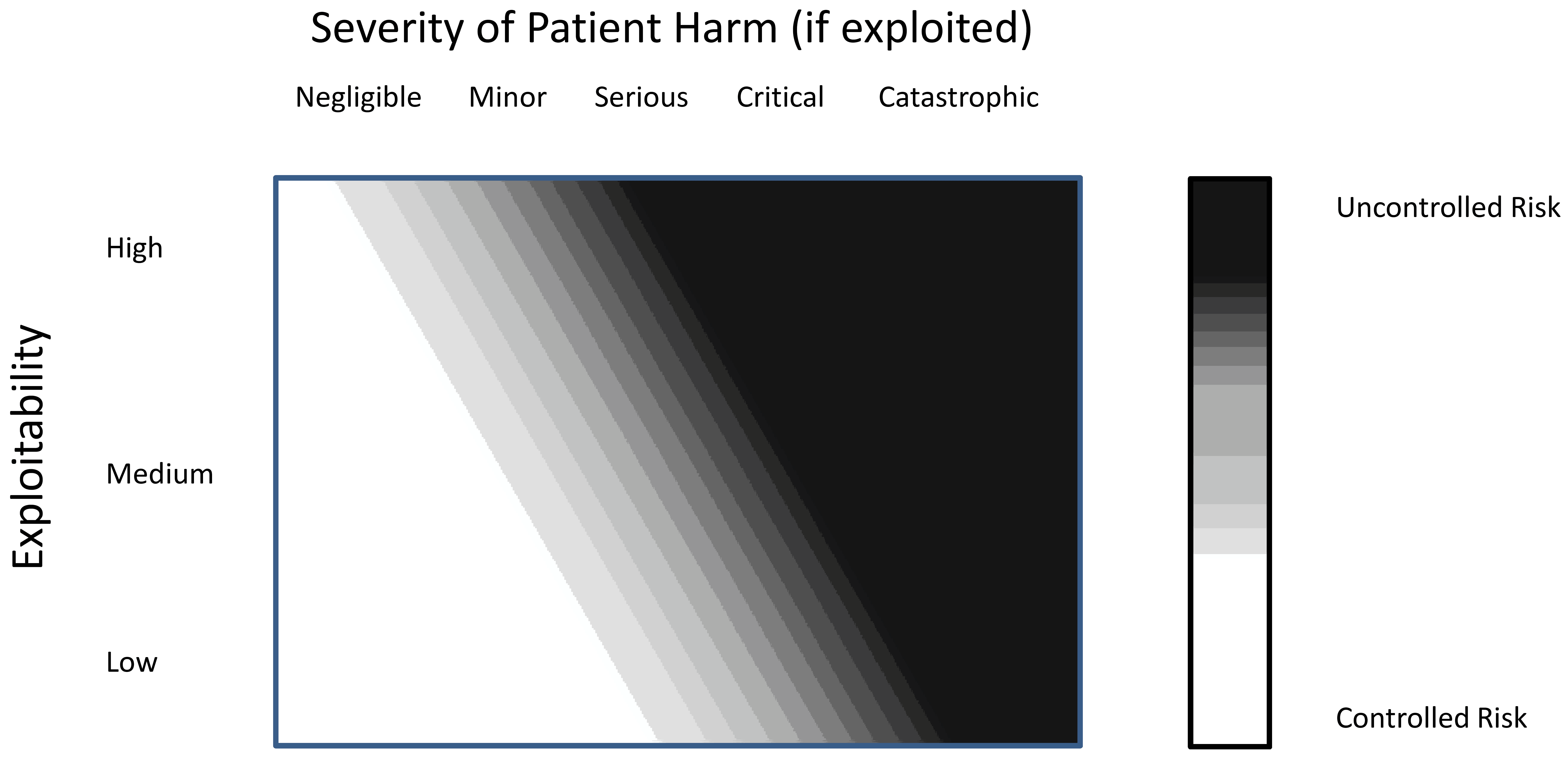
1. Inadequate Threat Modeling and Risk Assessment 🔗
One of the most frequent objections from FDA relates to incomplete or inadequate threat modeling and risk assessment. FDA expects manufacturers to consider a wide range of potential threats and evaluate their impact on device safety and effectiveness.
A typical objection in this area might read:
"Threat model and risk assessment documentation is incomplete, not evaluating risks from all relevant threat sources."
These objections highlight a common pattern: manufacturers often focus on obvious or likely threats while overlooking less apparent but potentially significant risks.
Best Practices:
- Conduct comprehensive threat modeling that considers external attackers, insider threats, supply chain risks, and environmental factors.
- Use structured methodologies like STRIDE or PASTA to ensure a thorough approach.
- Document your threat modeling process and results clearly, showing how each identified threat is addressed.
2. Insufficient Authentication and Authorization Controls 🔗
FDA places significant emphasis on robust authentication and authorization mechanisms to prevent unauthorized access to devices and sensitive data.
A common objection in this area is:
"Include cybersecurity functions, including authorization controls, in the device; specifically, this guidance recommends that device manufacturers employ, where appropriate, a layered authorization model by differentiating privileges based on the user role (e.g., caregiver, system administrator) or device role."
Another related objection states:
"Authorization controls: specifically, you have not defined your approach to authorization and user privilege."
These objections reflect a pattern where manufacturers may implement basic authentication but fail to provide granular, role-based access controls.
Best Practices:
- Implement multi-factor authentication where appropriate.
- Develop a layered authorization model with clearly defined user roles and privileges.
- Apply the principle of least privilege to minimize potential damage from compromised accounts.
- Document your authentication and authorization scheme thoroughly, explaining the rationale behind your choices.
3. Weak Encryption and Data Protection Measures 🔗
Data protection is a critical aspect of medical device security, and FDA scrutinizes the encryption and data protection measures implemented in devices.
A typical objection might state:
"Ensure the capability of secure data transfer to-and-from the device and, when appropriate, use encryption methods—because inadequate confidentiality controls can lead to the exposure of authentication protocol keys, passwords, and information or commands transmitted to or from the device whose plaintext form could expose commands or information which could be used to impact device safety and effectiveness."
Another related objection is:
"Confidentiality Controls: describe control implementation for securing data transfer to-and-from the device, and for encryption algorithms, provide a detailed justification for how the algorithm(s) may offer sufficient security based on the risk of the asset."
These objections often emerge when manufacturers fail to implement strong encryption or don't provide sufficient justification for their chosen methods.
Best Practices:
- Use industry-standard encryption algorithms and protocols.
- Implement robust key management practices.
- Protect data both in transit and at rest.
- Provide detailed documentation on your encryption implementation, including algorithm choices and key management procedures.
- Justify the security of your chosen algorithms based on the risk profile of your device and the sensitivity of the data being protected.
4. Inadequate Software Bill of Materials (SBOM) 🔗
FDA has increasingly emphasized the importance of providing a comprehensive Software Bill of Materials (SBOM) to understand the software components used in a device and their associated risks.
A common objection in this area is:
"you did not provide a software bill of materials (SBOM), including commercial, open-source, and OTS software components as required by section 524B(b)(3) of the FD&C Act."
Another related objection states:
"the documentation is not adequate because it did not fully describe the complete set of software functions including information on operating system and other OTS software."
These objections often occur when manufacturers overlook the SBOM requirement or provide incomplete information about third-party and off-the-shelf (OTS) software components.
Best Practices:
- Maintain a comprehensive SBOM that includes all software components, including third-party and open-source software.
- Use industry-standard formats like SPDX or CycloneDX for your SBOM.
- Regularly update the SBOM as software components change.
- Provide clear documentation on how you manage and mitigate risks associated with third-party software components.
- Include detailed information about the operating system and other OTS software used in your device.
5. Insufficient Update and Patch Management 🔗
FDA expects manufacturers to have robust processes for developing, testing, and deploying software updates and security patches throughout the device lifecycle.
A typical objection might read:
"However, you did not provide adequate information timelines to release updates and patches."
This objection pattern often emerges when manufacturers fail to provide detailed information on their update and patch management processes.
Best Practices:
- Develop a comprehensive software update and patch management process.
- Establish clear timelines for developing and deploying critical security updates.
- Implement secure update mechanisms that verify the authenticity and integrity of updates.
- Document your update and patch management procedures, including testing processes and deployment strategies.
6. Inadequate Logging and Monitoring 🔗
FDA expects devices to have robust logging and monitoring capabilities to detect and respond to security events.
A common objection in this area is:
"it is not clear how the device detects, monitors, logs, and/or alerts users of security compromise. You listed some general means by which cybersecurity signals can be detected, however, you did not provide specific information on how these events are detected through internal investigations."
This objection pattern often occurs when manufacturers provide vague or incomplete information about their logging and monitoring capabilities.
Best Practices:
- Implement comprehensive logging of security-relevant events.
- Develop clear procedures for monitoring logs and detecting potential security incidents.
- Implement automated alerting mechanisms for critical security events.
- Document your logging and monitoring processes in detail, including what events are logged, how logs are protected, and how they are analyzed.
7. Lack of Device Hardening Measures 🔗
FDA expects manufacturers to implement appropriate hardening measures to reduce the attack surface of their devices.
A typical objection might state:
"Appropriate hardening includes but may not be limited to removal of unused software and code, removal of debug code, removal of hardcoded or default passwords, removal or permanent disablement of unused functionality like network ports and communication interfaces (i.e., Bluetooth, Wi-Fi, etc.), removal of autorun functionality on hardware ports (e.g., USB ports), and restriction of read/write permissions based on authorization level."
Another related objection is:
"you did not provide adequate information on hardening controls used to protect the device. Specifically, you have not broached or discussed the concept of hardening."
These objections often emerge when manufacturers fail to implement or document comprehensive hardening measures.
Best Practices:
- Develop a thorough device hardening process that addresses all aspects mentioned in FDA's guidance.
- Regularly review and update your hardening procedures as new best practices emerge.
- Document your hardening process in detail, explaining the rationale behind each measure.
- Conduct regular vulnerability assessments to ensure the effectiveness of your hardening measures.
8. Insufficient Consideration of Third-Party and Legacy Components 🔗
FDA pays close attention to how manufacturers manage risks associated with third-party components and legacy systems.
A common objection in this area is:
"indicate that at least one of the computers controlling a hardware operation is using Microsoft Windows as the operating system (OS) for the device. You have not indicated the version of this OS, nor have you indicated the OS for the other computers that control a separate hardware operation. Therefore, it is not known when one or more OS components in your device will reach and pass its end of support date and if your device is expected to be in use at that time."
This objection pattern often occurs when manufacturers fail to provide comprehensive information about all software components used in their devices, especially off-the-shelf (OTS) and legacy components.
Best Practices:
- Maintain a comprehensive inventory of all software components, including third-party and legacy systems.
- Conduct thorough risk assessments for all components, particularly those that are no longer supported by their vendors.
- Develop mitigation strategies for risks associated with legacy components that cannot be easily updated or replaced.
- Provide detailed documentation on how you manage and mitigate risks associated with third-party and legacy components.
- Clearly identify the versions of all operating systems and other software components used in your device.
9. Inadequate Decommissioning Procedures 🔗
FDA expects manufacturers to have secure procedures for decommissioning devices at the end of their lifecycle.
A typical objection might read:
"Information on securely decommissioning devices by sanitizing the product of sensitive, confidential, and proprietary data and software."
This objection pattern often emerges when manufacturers fail to address the security implications of device end-of-life.
Best Practices:
- Develop comprehensive decommissioning procedures that address data sanitization and secure disposal of hardware.
- Implement secure data wiping techniques that meet industry standards.
- Document your decommissioning procedures, including methods for verifying successful data sanitization.
- Consider the entire device lifecycle in your cybersecurity planning, from initial deployment through decommissioning.
10. Insufficient Cybersecurity Testing 🔗
FDA expects manufacturers to conduct thorough cybersecurity testing to validate the effectiveness of their security controls.
A common objection in this area is:
"Lack of systematic and rigorous cybersecurity testing, including techniques like static/dynamic code analysis, fuzz testing, vulnerability testing, and penetration testing."
Another related objection states:
"However, it appears that the testing did not include requirement verification, static and dynamic code analysis, and malformed input (fuzz) testing."
These objections often occur when manufacturers rely solely on functional testing and fail to implement comprehensive security-specific testing.
Best Practices:
- Develop a comprehensive cybersecurity testing strategy that includes a range of techniques such as static and dynamic analysis, fuzz testing, and penetration testing.
- Integrate security testing throughout the development process, not just at the end.
- Use both automated tools and manual testing methods to identify potential vulnerabilities.
- Document your testing procedures and results thoroughly, explaining how each identified vulnerability is addressed.
- Include requirement verification as part of your testing process to ensure all security requirements are met.
11. Inadequate Cloud Service Management 🔗
For devices that rely on cloud services, FDA expects manufacturers to have robust plans for handling potential cloud outages and ensuring data security in cloud environments.
A typical objection in this area might read:
"it appears your device relies upon cloud capabilities to perform aspects of the intended use. However, it is not clear what plans/operations are in place for the device should the cloud-based service be unavailable."
This objection highlights the need to address potential disruptions in cloud services and their impact on device functionality.
Best Practices:
- Clearly describe your cloud infrastructure and dependencies.
- Conduct a thorough risk assessment of potential cloud outages and their impact on device functionality and patient safety.
- Develop and document contingency plans for handling cloud service disruptions.
- Implement and test failover mechanisms to ensure device functionality during cloud outages.
- Consider implementing a multi-cloud strategy to enhance resilience.
12. Insufficient Labeling and User Guidance 🔗
FDA expects manufacturers to provide clear and comprehensive cybersecurity labeling and user guidance to ensure users can operate devices securely.
A common objection in this area is:
"you did not provide cybersecurity labeling; the location indicated in your eSTAR submission please provide the following:
- A description of all interfaces and communication protocols available on the device.
- Instructions on how to maintain the device cybersecurity and how to update the firmware / software for the device.
- Instructions for any security actions that the user or user facility are expected to take or implement to ensure secure use of the device.
- Inform users of any network or connection dependencies that might be intentionally disabled and therefore unavailable to the users.
- Include a description of cybersecurity events that can be detected by the device and a description of how users will be informed of such events.
- Include instructions for what a user should do if a cybersecurity event is detected or suspected (i.e., incident response plan)."
This objection highlights the need for comprehensive cybersecurity information in device labeling and user documentation.
Best Practices:
- Develop clear and detailed cybersecurity labeling that addresses all points mentioned in FDA's objection.
- Provide user-friendly instructions for maintaining device cybersecurity and applying updates.
- Clearly communicate any security actions that users are expected to take.
- Document all device interfaces, communication protocols, and network dependencies.
- Provide guidance on identifying and responding to potential cybersecurity events.
13. Inadequate Management of Unresolved Anomalies 🔗
FDA expects manufacturers to carefully assess and document any unresolved software anomalies, including their potential impact on device security.
A typical objection in this area might state:
"Cybersecurity risk evaluation is incomplete as Unresolved Anomalies were not assessed for cybersecurity impacts as part of the risk assessment and threat modeling."
This objection highlights the need to consider the security implications of all software anomalies, even those that may seem primarily functional in nature.
Best Practices:
- Maintain a comprehensive list of all unresolved software anomalies.
- Conduct a thorough security risk assessment for each unresolved anomaly.
- Document the potential impact of each anomaly on device security and functionality.
- Develop and document mitigation strategies for any anomalies that pose security risks.
- Provide clear justification for any anomalies that will remain unresolved in the marketed device.
14. Insufficient Consideration of AI/ML Algorithms 🔗
For devices that incorporate artificial intelligence (AI) or machine learning (ML) algorithms, FDA expects thorough validation and documentation of these components.
A relevant objection in this area is:
"You are seeking clearance of a device that uses machine learning algorithm(s) as part of its key functionality. You have provided a high-level summary of performance data. However, this summary does not contain details on validation of the deep learning algorithm."
This objection highlights the need for detailed validation of AI/ML components in medical devices.
Best Practices:
- Provide detailed descriptions of any AI/ML algorithms used in your device.
- Document the training data used for these algorithms, including its size, diversity, and quality.
- Describe your validation methods and metrics for evaluating algorithm performance.
- Explain how you've addressed potential biases in your AI/ML algorithms.
- Provide clear documentation on how AI/ML components are integrated into the overall device functionality and security architecture.
Key Takeaways 🔗
- Comprehensive Threat Modeling: Conduct thorough threat modeling that considers all potential sources of risk, including external attackers, insider threats, supply chain vulnerabilities, and environmental factors.
- Robust Authentication and Authorization: Implement strong, multi-layered authentication and authorization controls, including multi-factor authentication and role-based access control (RBAC) where appropriate.
- Strong Encryption Practices: Use industry-standard encryption algorithms and protocols for data protection, both in transit and at rest. Justify your choices based on your device's risk profile.
- Detailed Software Bill of Materials (SBOM): Maintain and provide a comprehensive SBOM that includes all software components, including third-party and open-source software. Keep this document updated throughout the device lifecycle.
- Rigorous Cybersecurity Testing: Conduct and document comprehensive cybersecurity testing, including static and dynamic code analysis, fuzz testing, vulnerability scanning, and penetration testing.
- Effective Update and Patch Management: Develop and document robust processes for timely development, testing, and deployment of software updates and security patches.
- Comprehensive Logging and Monitoring: Implement thorough logging and monitoring capabilities to detect, alert, and respond to potential security events.
- Device Hardening Measures: Apply and document comprehensive device hardening measures, including removal of unnecessary software, closure of unused ports, and implementation of least privilege principles.
- Legacy Component Management: Carefully assess and mitigate risks associated with legacy components that cannot be easily updated, documenting your approach for FDA review.
- Cloud Service Considerations: For cloud-dependent devices, clearly document your cloud infrastructure, assess potential outage impacts, and develop robust contingency plans.
- AI/ML Algorithm Validation: For devices incorporating AI or ML, provide detailed documentation on algorithm validation, training data, and measures to address potential biases.
- Lifecycle Management: Consider cybersecurity throughout the entire device lifecycle, from initial design through decommissioning, and document your approach for each phase.
- Clear User Guidance: Provide comprehensive, user-friendly cybersecurity labeling and instructions to ensure users can operate devices securely and respond appropriately to security events.
- Ongoing Cybersecurity Management: Develop and document a robust plan for ongoing cybersecurity management, including vulnerability monitoring, incident response, and coordinated disclosure procedures.
- Transparent Documentation: Provide clear, detailed documentation of all cybersecurity measures, risk assessments, and mitigation strategies in your FDA submissions. Transparency is key to a successful review process.
Conclusion 🔗
Navigating FDA's cybersecurity requirements for medical devices can be challenging, but understanding common objections, patterns, and best practices can significantly smooth the process. By taking a comprehensive, proactive approach to cybersecurity—from threat modeling and risk assessment through to ongoing management and incident response—manufacturers can not only meet regulatory requirements but also build truly secure devices that protect patient safety and privacy.
Remember, cybersecurity is not a one-time effort but an ongoing process that requires constant vigilance and adaptation. Stay informed about evolving threats and regulatory expectations, and be prepared to continuously improve your cybersecurity practices. By doing so, you'll be well-positioned to navigate the complex landscape of medical device cybersecurity and build trust with both regulators and end-users.
Revision History 🔗
| Date | Changes |
|---|---|
| 2024-08-07 | Initial Version |